Abstract
Background
Peripheral T-cell lymphomas (PTCLs) are a rare and heterogeneous group of lymphoid malignancies characterized by frequent relapse or progression and less than 30% 5-year overall survival. The treatment outcome is still unsatisfactory, and the majority of data about patients with PTCLs are from retrospective studies or small study population-based phase II studies. Thus the prospective study investigating treatment outcomes of patients with PTCLs in clinical practice is required for better understanding of PTCLs and their unmet needs in real world situation.
Methods
We have conducted a nationwide, multicenter, prospective registry study for patients with PTCL since April 2015. After written informed consent, patients receiving chemotherapy with curative content were registered and prospectively monitored [ClinicalTrials.gov Identifier: NCT02364466]. All patients were pathologically diagnosed with PTCLs according to World Health Organization Classification 2008. Extranodal NK/T cell lymphoma, and cutaneous T cell lymphoma, Mycosis fungoides and Sezary syndrome were excluded because of their different treatment strategy. The target number for enrollment was 200, and all patients' clinical data and survival status will be updated until the end of study (31th December 2019). The interim analysis was performed at the time of 155 patients were enrolled.
Results
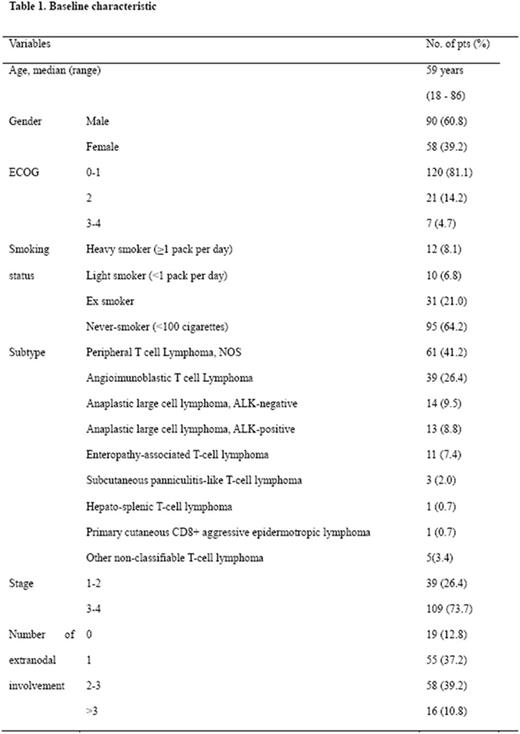
Among 155 patients, we analyzed the clinical features and treatment outcome of 148 patients. Median age was 59 years (range, 18 - 86). Ninety patients (60.8%) were male, and ECOG performance status was 0-1 in most patients (81.1%). PTCL, not otherwise specified was the most common pathologic subtype accounting for 41.2% (61 patients), and angioimmunoblastic T-cell lymphoma (39 patients, 26.4%) was followed. One hundred nine patients (73.7%) were presented as advanced stage disease, and extranodal spread was found in most patients (129 patients, 87.2%) (Table 1). The pattern of extranodal involvement was not different over pathologic subtypes, which most commonly involved sites were spleen (37 patients, 25.0%), and bone marrow (35 patients, 23.6%). CHOP or CHOP-like regimen was most frequently used as the 1st line treatment regimen (111 patients, 75.0%), ICE (16 patients, 10.8%) and others (21 patients, 14.2%) were followed. The final response to the 1st line chemotherapy was available in 100 patients, which ORR was 69.0% and CR rate was 48.0%. The ORR was not different between CHOP-treated and ICE-treated groups (ORR = 72.2% and 70.0%, p = 0.88), while CR rate was better in CHOP-treated group than in ICE-treated group (CR = 54.2% vs. 20.0%, p = 0.043). Among patients who started 1st line chemotherapy, 77 patients completed their planned 6 to 8 cycles of chemotherapy, while treatment schedule was interrupted due to disease progression or intolerance in 17 patients and 3 patients, respectively. A total of 31 patients were treated with various kinds of 2nd line chemotherapy after relapse or progression. The ORR and CR rate of salvage chemotherapy were 38.2% and 20.1%, respectively. Autologous hematopoietic stem cell transplantation was performed in 24 patients (16.2%) as an upfront consolidative treatment in 19 patients (79.2%) or a salvage treatment in 5 patients (20.8%). Median progression-free survival and overall survival were not reached yet due to the short follow-up duration (7.4 months). At the data cut-off time of July 12th 2017, twenty patients (13.5%) were dead and 14 patients were lost to follow-up. Among 20 patients who were dead, 14 patients died due to lymphoma progression, while the other 6 patients expired from lymphoma-unrelated causes.
Conclusions
Our study shows a prospective collection of clinical data about the treatment pattern and outcomes in patients with newly diagnosed PTCL in real world clinical practice. Our findings suggested that the clinical outcomes of the patients with PTCL in real world might be poorer than those of clinical trials. In particular, more effective treatment strategy for relapsed or refractory PTCL should be actively investigated considering the unmet needs proposed by the current study. A longer follow-up is needed to provide the detailed information about the treatment outcomes including treatment-related complications and survival.
Won Seog: Samsung Medical Center: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal